The idea of a virtual health assistant once conjured images of chatbots offering generic advice. In China, however, digital health has evolved into a sophisticated ecosystem that combines artificial intelligence (AI), telemedicine, cloud infrastructure, and regulatory reforms. In 2025, the country’s health‑tech landscape has become one of the most vibrant and complex in the world.
A vast population, uneven distribution of clinicians, rapid aging, and the COVID-19 Era’s digitization have accelerated the demand for technologies that can triage patients, guide chronic disease management, and support overstretched nursing staff.
This article explores how virtual health assistants and related technologies are reshaping China’s healthcare delivery system, drawing on case studies, academic research, and policy analysis.
Evolution of Virtual Health Assistants in China
Roots in Internet Hospitals and Enterprise‑led Platforms
China’s early foray into virtual health assistants began with internet hospitals—platforms where patients could consult doctors remotely. In 2015, the State Council’s “Internet Plus” action plan explicitly encouraged integration of internet technologies with healthcare.
Subsequent regulations in 2018 defined admission criteria and supervision mechanisms for internet medical institutions, while guidelines in 2020 allowed medical insurance to reimburse online consultations. This created fertile ground for enterprise-led platforms, such as Good Doctor Online, JD Health, and Ping An Good Doctor.
Scale and Limitations of Early Platforms
An extensive cross‑sectional study highlights the scale of these platforms. As of December 2022, over 149,000 doctors from 7,584 healthcare institutions have delivered more than 40 million online consultations, with senior or intermediate physicians (88% from tertiary hospitals) comprising the majority of the supply.
The median consultation price was approximately 49 RMB, indicating affordability compared to in-person visits. Common complaints included upper respiratory infections (16.19%), gynecological disorders (11.98%), and skin diseases (8.65%).
The age distribution peaked among individuals under five years and those aged 20–39 years. These statistics suggest that China’s virtual clinics initially focused on non-urgent, high-volume cases and younger users.
While enterprise‑led models improved access, they also created fragmentation. Early virtual assistants were essentially messaging platforms that connected patients with doctors rather than providing autonomous medical advice. Government-led internet hospitals (affiliated with county or city health commissions) and hospital-led platforms soon followed.
Still, enterprise offerings retained scale advantages due to their ability to mobilize big data and AI. The market matured when AI‑driven diagnostics and conversation agents were introduced, transforming virtual assistants from simple chatbots into clinical decision‑support tools.
Rise of AI Hospitals and LLM‑powered Assistants

In 2024, Tsinghua University launched the world’s first AI Agent Hospital, also known as Agent Hospital. Developed from the MedAgent-Zero system, this hospital initially ran with 14 AI doctors, later expanding to 42 AI doctors covering 21 medical specialties and 300 diseases. These AI doctors were trained on more than 500,000 synthetic patient cases, enabling them to deliver around 10,000 consultations daily with an accuracy rate of 93%.
The platform integrates digital admissions, predictive alerts, AI‑powered diagnostics, infusion management, and mobile nursing within Beijing Tsinghua Chang Gung Hospital. Unlike earlier pilots, the AI hospital embeds AI at the foundational design level rather than bolting algorithms onto existing workflows, illustrating a shift toward “AI‑collaborative physicians”.
In parallel with the AI hospital, open‑source medical large language models (LLMs) were deployed nationwide. DeepSeek, one of China’s most influential models, operates across more than 260 hospitals, spanning 93.5% of provinces.
DeepSeek performs tasks such as automated pathology slide analysis, rare disease screening, intelligent triage, and AI-generated medical documentation. Local intranet deployment ensures that patient data remains within hospital firewalls.
However, a cross-sectional survey revealed a national deployment rate of just 0.7%. Eighty-four % of deployments occur in tertiary hospitals, and the most advanced (671 B parameter) model is used for strategic decision-making, whereas smaller models support routine diagnosis. These statistics highlight the disparity between cutting-edge institutions and rural or primary care facilities, an issue that policymakers must address.
AI‑Driven Diagnostics and Triage

Enhancing Clinical Accuracy and Efficiency
The promise of AI-driven diagnostics lies in its ability to process vast datasets quickly and provide clinicians with decision support. The AI Agent Hospital demonstrates how synthetic patient cases and reinforcement learning can train algorithms to recognize patterns across diverse diseases.
It’s 42 AI doctors deliver consultations covering 21 specialties, using digital tools to integrate patient history, imaging, pathology, and lab results into a comprehensive assessment. According to Tsinghua University, this system is designed to complement clinicians rather than replace them; physicians oversee AI recommendations and make final diagnoses and treatment plans.
For hospital administrators, this integrated approach promises lower operational costs, improved patient satisfaction, and a more effective response to specialist shortages.
DeepSeek provides another example of AI‑augmented diagnostics. At Ruijin Hospital, DeepSeek’s computer vision analysis processes more than 3,000 pathology slides per day, significantly accelerating diagnosis and reducing human error.
Chengdu First People’s Hospital uses DeepSeek to deliver telemedicine for remote consultations, while Shanghai Sixth People’s Hospital integrates the LLM into real‑time AI workstations for clinical documentation. Despite these successes, adoption remains limited, with only 0.7% of hospitals nationwide having implemented these models, reflecting challenges with cost, integration, and regulatory compliance.
Challenges of Integration and Data Quality
Deploying AI diagnostics in Chinese hospitals requires a robust IT infrastructure, high-quality electronic medical records, and interdisciplinary collaboration.
A 2025 study found that tertiary hospitals that incorporated DeepSeek experienced significant improvements in diagnostic accuracy and efficiency; however, integration required upgrades to network security, computing capacity, and data management practices.
Clinicians require training to effectively interpret AI recommendations and integrate them into their existing workflows.
Moreover, data privacy concerns remain; although DeepSeek’s local deployment protects information, hospitals must ensure that algorithms do not introduce bias or inadvertently reveal sensitive data.
The disparity between economically developed regions and rural areas further complicates the adoption process. DeepSeek deployments are concentrated in central, eastern, and northern China, leaving remote hospitals with limited access to AI. The central government and provincial health commissions thus face the challenge of scaling AI across diverse healthcare settings while ensuring fairness and quality control.
Virtual Nursing and Elderly Care

Addressing Workforce Shortages and Aging
China’s population is aging rapidly, with those aged 60 and older expected to comprise more than 30% of the total by 2035. At the same time, the World Health Organization warns of a global shortage of 4.5 million nurses by 2030. Chinese nurses already experience heavy workloads; thus, virtual nursing assistants and robots are being explored to fill the gap.
A cross-sectional study at Wuhan Asia Heart Hospital surveyed 457 visitors regarding their expectations for AI nursing robots. Hospitalized visitors prioritized functions supporting medical activities (monitoring vital signs, delivering medication), while outpatient visitors valued treatment assistance, and those seeking companionship emphasized psychological and life support.
This suggests that AI nursing robots must be tailored to specific contexts, such as hospital clinical support and home-based social support.
Case Study: Nurabot%, cut physical fatigue,
Though developed in Taiwan, Nurabot illustrates the potential of AI nursing robots for Chinese hospitals. Built by Foxconn and NVIDIA, Nurabot utilizes digital twin simulations of hospital wards to train its AI and perform tasks such as delivering medicine, conducting ward patrols, and guiding visitors.
Foxconn claims the robot can reduce nurse workloads by 30%, cut physical fatigue, and allow nurses to focus on patient interactions. While the Chinese mainland has not widely adopted Nurabot specifically, similar concepts are being piloted in major hospitals and elder‑care facilities.
The Taiwan example demonstrates that robotics, combined with AI, can automate labor-intensive tasks, streamline logistics, and enhance the patient experience.
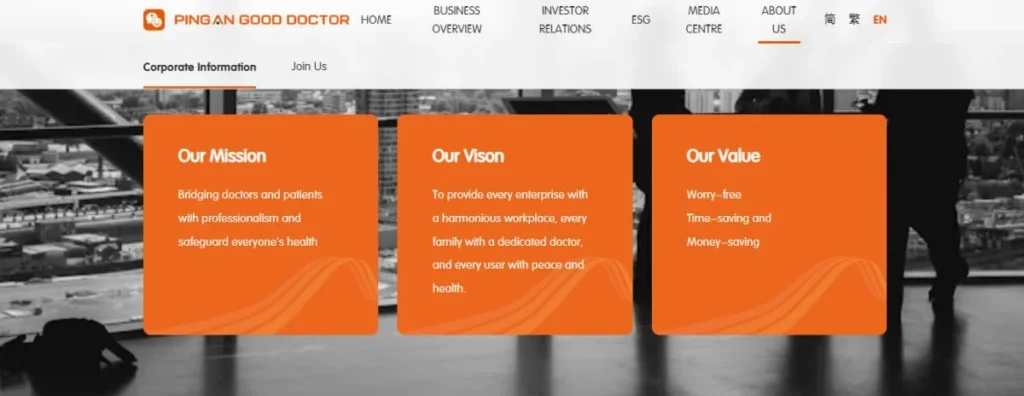
Ping An Good Doctor’s AI Senior Care
Virtual nursing is not limited to robots; digital avatars and voice‑based assistants provide companionship and health monitoring for older adults living at home. Ping An Good Doctor, one of China’s largest healthcare platforms, reported that its family doctor membership exceeded 35 million and that users of its home‑based senior‑care services increased by 83 % year‑on‑year across 85 cities.
The company partners with over 4,000 hospitals, 106,000 health service providers, 240,000 pharmacies, and 100 senior‑care institutions, enabling it to offer a comprehensive support network.
Its “7+N+1” AI product system includes a digital avatar that can interact with patients, an AI family doctor for primary care, an AI senior‑care concierge, and an AI health manager.
Using data from 1.44 billion consultations, the platform’s AI consultation accuracy reached 98%, multidisciplinary treatment plan accuracy reached 80%, and daily service capacity reached 4 million visits.
These capabilities translate into tangible benefits: Ping An reduced the average service cost per family doctor user by 52% and improved operational efficiency by approximately 50%. For investors and executives, these numbers demonstrate the commercial viability of AI‑enabled virtual nursing and the potential to scale it domestically and internationally.
Optimizing Robots for Human Acceptance
The adoption of AI nursing robots depends not only on technical capabilities but also on public acceptance and ethical considerations. The Wuhan study notes that psychological and life‑support functions are crucial for visitors who need companionship, indicating that robots should be designed with empathy and interactive capabilities.
Additionally, the study emphasizes that older adults may require simple interfaces and family engagement to alleviate concerns about feelings of abandonment. Developers must thus prioritize user-centered design and cultural sensitivity when introducing virtual assistants into Chinese healthcare settings.
Telemedicine Integration and Virtual Hospitals
Hybrid Models Combining AI and Telehealth
Telemedicine platforms are increasingly integrated with AI to provide seamless patient journeys. The enterprise‑led Good Doctor Online platform demonstrates how large volumes of consultations can generate data for AI training.
Doctors using the platform were predominantly from tertiary hospitals, and most consultations involved common conditions. However, AI triage and automated follow-ups can extend the service to chronic disease management, mental health support, and remote patient monitoring in rural areas.
DeepSeek plays an essential role in these hybrid models. Its local deployment ensures data security, while its large language model capabilities enable natural language dialogue, summarization of patient records, and triage recommendations.
Hospitals such as Chengdu First People’s Hospital integrate DeepSeek into their telemedicine systems, connecting rural clinics with urban specialists. By cross-referencing patient symptoms with up-to-date medical literature, AI can suggest probable diagnoses and advise whether patients should visit a hospital or continue with home care.
Digital Hospitals and Smart Infrastructure
The AI Agent Hospital at Beijing Tsinghua Chang Gung is both a physical hospital and a digital platform. Its design integrates AI throughout the patient journey: digital admissions reduce paperwork, predictive alerts notify nurses when patient vital signs deviate, and infusion management and mobile nursing improve the efficiency of care delivery.
The hospital expanded its capacity to 1,500 inpatients and 10,000 outpatients, partly due to AI-enabled process optimization. Such digital hospitals are prototypes for future smart infrastructure—physical spaces that seamlessly connect to virtual assistants and allow remote consultations, tele‑ICU monitoring, and AI‑driven diagnostics.
Insurance Coverage and Pricing Models
The government’s 2020 policy, which permits medical insurance reimbursement for online consultations, has been pivotal in the adoption of telemedicine. Nevertheless, pricing models remain inconsistent; the Good Doctor study found wide variability in consultation fees across specialties and cities.
Policymakers aim to standardize pricing to avoid inequity and ensure fairness. The expansion of commercial health insurance also supports virtual care, with insurers covering online consultations, AI diagnosis, and chronic disease management, thereby encouraging more patients and providers to embrace digital services.
Healthcare Infrastructure and Investment
Building the Digital Backbone
Effective virtual health assistants rely on robust infrastructure, including high‑speed internet, interoperable electronic health records (EHRs), cloud computing, and cybersecurity protocols. Hospitals introducing DeepSeek or AI agent systems must upgrade their servers, data storage, and network security to handle the large computational loads and ensure patient privacy is maintained.
Data quality is another critical factor; fragmented or inaccurate records can impair AI performance and lead to misdiagnoses. Thus, hospitals are investing in data cleaning, standardization, and real‑time data capture technologies.
Because China’s healthcare system is decentralized, infrastructure investment varies by region. Economic powerhouses such as Beijing, Shanghai, and Guangdong have quickly adopted digital health, while less developed provinces lag.
Public–private partnerships are therefore essential. Tech giants such as Tencent, Alibaba, and Baidu invest in cloud services and AI platforms, while local governments finance the expansion of broadband and the development of health information exchanges. These partnerships can accelerate the scaling of virtual health assistants to rural and community health centers.
The Investment Landscape
Digital health has emerged as a significant investment theme in China. Ping An Good Doctor, for example, raised billions through its initial public offering and subsequent financing rounds.
According to its mid-2025 report, the platform employs approximately 50,000 in-house and contracted doctors across 37 specialties and operates partnerships with tens of thousands of healthcare providers. The growth of home-based senior care services (an 83 % year-on-year increase) signals strong demand for virtual assistants among older adults.
Investors are also backing start-ups that develop AI-powered nurses, virtual therapists, and apps for managing chronic diseases. The success of DeepSeek—deployed in over 260 hospitals with local intranet installation—shows that open‑source models can achieve scale when combined with commercial services.
However, early‑stage companies face regulatory hurdles and require compliance expertise to navigate health data laws. Venture capital funds are therefore partnering with legal consultants and former regulators to mitigate risk.
Challenges and Limitations
While virtual health assistants offer transformative potential, numerous challenges must be addressed:
- Data Privacy and Security: Strict regulations protect personal data, but frequent updates and overlapping laws can create compliance burdens for hospitals and start‑ups. Ensuring anonymization, consent management, and secure storage requires significant investment.
- Integration Complexity: Incorporating AI assistants into existing clinical workflows demands system interoperability, data standardization, and staff training. Some hospitals struggle with outdated IT systems and a lack of technical expertise.
- Access and Equity: Only 0.7% of hospitals have deployed large models, such as those found on DeepSeek. Rural areas often lack the necessary infrastructure to support AI, thereby exacerbating existing disparities.
- Ethical and Legal Accountability: As AI takes on diagnostic and treatment recommendations, questions arise about liability when errors occur. Current regulations require physicians to assume final responsibility, but this may evolve as AI autonomy increases.
- Cultural Acceptance: AI nursing robots must be designed to align with patient expectations. Research shows that visitors value psychological support and companionship as much as medical assistance; therefore, overly technical designs could lead to rejection.
- Reliability and Bias: AI algorithms are only as good as the data they are trained on. Biases in data sets can lead to misdiagnoses, especially in minority populations. Continuous validation and updating are therefore essential.
Future Outlook: 2025 and Beyond
Convergence of AI, Wearables, and Smart Homes
Looking ahead, virtual health assistants will extend beyond hospitals and mobile apps into smart homes. Wearable sensors and Internet of Things (IoT) devices will feed real‑time data to AI systems, enabling proactive health management.
For elderly patients, home‑based virtual assistants may monitor heart rate, sleep patterns, and medication adherence, alerting caregivers when anomalies occur. China’s Ministry of Industry and Information Technology has partnered with tech companies to develop “Healthy Home” standards that integrate medical devices with home automation, ensuring interoperability and compliance.
Generative AI and Personalized Medicine
The next generation of virtual assistants will leverage generative AI to provide personalized medical advice. Instead of preprogrammed scripts, models will synthesize medical literature, patient history, and social determinants to deliver bespoke recommendations.
Developers are experimenting with voice‑activated assistants that speak regional dialects, making technology accessible to seniors and rural residents. In oncology, AI assistants can design personalized treatment regimens by analyzing tumor genomics, while in mental health, they may provide cognitive behavioral therapy or connect patients with counselors. Such advances will require rigorous validation and regulatory approval.
Expanded Regulatory Frameworks
As technologies evolve, policymakers will refine governance frameworks. We anticipate the development of more detailed standards for AI algorithm transparency, auditing, and certification.
International collaboration will also become increasingly important as Chinese companies deploy virtual assistants abroad and as foreign firms enter the Chinese market. Harmonizing data protection standards with global norms (e.g., GDPR) could facilitate cross‑border collaboration and innovation while safeguarding privacy.
Opportunities for Stakeholders
Healthcare executives should invest in digital infrastructure, including secure data platforms and staff training, to enhance patient care and improve operational efficiency. Digital health investors can look to companies like Ping An Good Doctor and start‑ups developing AI nursing robots or chronic disease management platforms.
Policymakers must strike a balance between innovation and patient protection, updating laws to accommodate emerging technologies. Medical professionals should engage in the development and validation of AI tools, ensuring clinical relevance and safety.
Ultimately, tech developers should prioritize user-centered design, data quality, and ethical considerations, collaborating closely with clinicians to develop trustworthy and effective systems.
Understand China’s Digital Health Revolution with Ashley Dudarenok
As China redefines healthcare through AI hospitals, virtual assistants, and large language models, the real opportunity lies in understanding how these systems reshape patient trust, care delivery, and data governance.
Ashley Dudarenok—China digital transformation expert, entrepreneur, and keynote speaker—helps global executives, investors, and healthcare innovators decode this transformation. Through her keynotes, research sessions, and executive workshops, Ashley provides rare insight into:
- How China’s “AI hospital” model is influencing the global healthcare tech race
- What investors can learn from platforms like Ping An Good Doctor and DeepSeek.
- How regulatory, cultural, and digital shifts in China are setting new global standards in telehealth and virtual care
Ashley has advised Fortune 500 companies, healthcare innovators, and policy leaders on adapting to China’s rapidly evolving tech ecosystem.
If your team wants to anticipate the next steps for virtual health and AI in medicine in China, book a consultation or keynote with Ashley Dudarenok today.
Frequently Asked Questions About Virtual Health Assistants in China
1. How do Virtual Health Assistants improve patient-doctor communication in China?
Virtual Health Assistants streamline communication by providing a structured symptom-collection process before patients meet with doctors. This reduces misunderstandings, saves time during consultations, and ensures physicians receive organized clinical details.
Many Chinese hospitals report shorter consultation times and higher patient satisfaction when AI tools act as a “bridge” for communication, especially for first-time visits.
2. What role do VHAs play in mental health support in China?
While still emerging, VHAs are increasingly used to provide early mental health screening and guidance. They can detect stress or depression patterns in chat-based interactions, offering self-care resources before referral to specialists.
This matters in China, where stigma sometimes prevents people from seeking psychiatric help directly. VHAs create an accessible first step for younger patients in particular.
3. How are VHAs supporting rural healthcare access?
In rural China, limited hospital staff and travel barriers slow down access to care. VHAs connected to internet hospitals help villagers conduct basic health assessments, request e-prescriptions, and receive remote follow-up instructions. This reduces unnecessary trips to urban hospitals and eases the burden on underfunded county clinics, making care more equitable across regions.
4. Can VHAs reduce healthcare costs for families?
Yes, VHAs can reduce costs by eliminating unnecessary in-person visits, shortening diagnostic timelines, and referring patients to appropriate specialists.
For patients with chronic diseases, medication reminders and lifestyle coaching help prevent complications that would otherwise require costly hospitalizations. Surveys show urban families appreciate the affordability of online consultations supported by VHAs compared to traditional outpatient visits.
5. How do VHAs affect the workload of Chinese doctors?
Doctors in China often face heavy patient loads, especially in tertiary hospitals. VHAs help by handling routine tasks like symptom triage, prescription refills, and follow-up reminders. This allows doctors to focus on complex cases requiring human expertise. Many tertiary hospitals report noticeable improvements in efficiency since integrating conversational AI into daily workflows.
6. Are Chinese patients comfortable sharing health data with VHAs?
Patient trust varies. Urban younger users are more open to digital interactions, while older patients may hesitate. Government rules on data sovereignty and privacy have improved confidence, especially with platforms backed by state or hospital systems. Still, transparency and clear consent processes are vital for sustained adoption across demographics.
7. Do VHAs in China integrate with wearable devices?
Yes, integration is growing quickly. VHAs link with smartwatches and health-monitoring devices to collect real-time data such as heart rate, glucose levels, and sleep patterns. This data supports chronic disease management programs and early detection of risks. Platforms like JD Health already use wearables to enhance adherence monitoring in diabetes and hypertension care.
8. How do VHAs handle China’s aging population challenges?
VHAs are being designed to support elderly users with medication reminders, simplified language interfaces, and integration with home monitoring systems. For example, AI assistants in eldercare facilities can track vitals and alert caregivers to sudden changes. This is particularly relevant as China’s 65+ population is expected to exceed 400 million by 2035.
9. Can VHAs provide multilingual support in China?
Yes, some platforms now offer Mandarin, Cantonese, and even minority languages. This improves access to healthcare for ethnic groups and migrant workers who may face language barriers. For international patients seeking care in China, English-language VHA options are also being developed to attract medical tourism and facilitate cross-border healthcare collaboration.
10. How do VHAs impact pharmaceutical distribution?
VHAs in China often connect directly to online pharmacies. After AI-assisted triage or consultation, patients can receive prescriptions and order medications through the same app. This streamlines the supply chain, reduces counterfeit risk, and supports better medication adherence by offering home delivery and digital reminders.
11. Are VHAs used in Chinese workplace healthcare programs?
Yes, large companies integrate VHAs into employee wellness platforms. Workers can access daily health check-ins, stress assessments, or chronic disease support without leaving the office. This reduces absenteeism and helps employers address rising health costs. In tech hubs like Shenzhen, corporate VHA adoption is part of broader workplace digital health strategies.
12. How are VHAs shaping medical education in China?
Medical schools and teaching hospitals use VHAs to train young doctors on triage and patient communication. AI agents simulate patient interactions, exposing students to a wide range of cases before clinical rotations. This helps address uneven training quality across provinces and builds familiarity with digital-first healthcare tools expected in future practice.
13. Do VHAs contribute to early disease detection in China?
Yes, VHAs analyze patient inputs and wearable data to identify red flags for conditions such as hypertension, diabetes, and respiratory infections. Early alerts allow patients to seek intervention before problems escalate. Pilot programs show improved detection rates in community clinics, where doctors previously struggled with limited screening resources.
14. How are VHAs influencing health insurance in China?
Insurers are starting to cover VHA consultations as part of digital health packages. This reduces claim costs by preventing hospital admissions through better chronic disease management. Some insurers even offer lower premiums to customers who actively engage with VHAs, rewarding preventive behavior and data sharing that improves overall risk profiling.
15. What challenges remain for widespread VHA adoption in China?
Challenges include uneven digital literacy among older populations, potential mistrust of AI-driven advice, and concerns over data misuse. Infrastructure gaps in rural areas also slow adoption. Success will depend on government support, strong regulatory safeguards, and patient education campaigns to ensure VHAs become trusted companions rather than optional digital add-ons.